Last week Alnylam reported positive news on Phase 3 outcomes for their RNA interference (RNAi) therapy to treat patients with a rare genetic cause of amyloidosis with polyneuropathy (see here). I tweeted the following:

The 20-year journey from scientific discovery to positive Phase 3 clinical trial data got me thinking about other novel therapeutic modalities. Was twenty years a long time or typical for an innovative therapeutic modality? Where are other promising modalities on their journey to regulatory approval? Is the biopharmaceutical industry on the cusp of a series of innovative modalities that could change the therapeutic landscape for patients? How will these new modalities improve our ability to test therapeutic hypotheses?
[Disclaimer: I am an employee of Celgene. The views expressed here are my own.]
To explore these questions, I decided to review different novel therapeutic modalities, which I am defining as those other than small molecules, protein therapeutics (e.g., insulin) and traditional vaccines. This decision was practical, as the amount of literature in these modalities is expansive.
For each new modality, I asked whether a drug has been approved by either a European or US regulatory agency (EMA and FDA, respectively). If a drug has been approved, I reviewed the time from seminal scientific discovery (which sometimes is clear, sometimes is not) to the approved therapy. I also asked how many other drugs have been approved within that same modality class, and the timing of approval for those drugs relative to the first drug in the class. If a drug in a new modality has not yet been approved, then I looked at a few recent events as a proxy for enthusiasm for the modality.
Here are my findings, which are followed by a few key takeaways.
A brief summary of novel therapeutic modalities with a drug approved by regulatory authorities.
I start with a chart of the modalities, date of seminal scientific discovery, date of regulatory approval, name / indication for first approved therapy, and the number of approval since the first one. Note that several of these categories overlap. For example, cellular therapy really includes CAR-T, ex vivo gene therapy, and oncolytic viruses.
| therapeutic modality | seminal discovery | regulatory approval | first approved therapy (brand name) | indication | No. approvals since first |
| monoclonal antibodies | 1975 | 1986 | Muromonab (Orthoclone OKT3) | transplant rejection | many |
| antisense oligonucleotide | 1978 | 1998 | Fomivirsen (Vitravene) | CMV retinitis | 3 |
| viral gene therapy | 1972 | 2012 | Alipogene tiparvovec (Glybera) | lipoprotein lipase deficiency | 0 |
| oncolytic viruses | 1960’s | 2015 | Talimogene laherparepvec, or “T-Vec” (Imlygic) | melanoma | 0 |
| cellular immunotherapy | 1973 | 2015 | Sipuleucel-T (Provenge) | prostate cancer | 0 |
| ex vivo gene therapy | 1972 | 2016 | Strimvelis | SCID | 0 |
| CAR-T therapy | 2005 | 2017 | Tisagenlecleucel (Kymriah) | B-cell ALL | 0 |
| RNAi | 1998 | pending | N/A | amyloidosis | N/A |
Monoclonal antibodies (mAb) – The technology to produce mAb was developed by Köhler & Milstein in 1975, who won the Nobel Prize in 1984. The first approved drug was just 11 years later, in 1986 (anti-CD3 [muronomab, or OKT3] for transplant rejection). But over the course of the next 10 years, only one additional mAb was approved (abciximab). The third mAb was rituximab (1997), thirteen years after the initial approval of muronomab. This success, however, was followed quickly in the next five years by approximately 10 additional mAb therapies for cancer, autoimmune and infectious diseases. The technology to generate mAbs continues to improve. Now there are many permutations on the mAb theme (e.g., bi-specific antibodies, bi-valent antibodies, nanobodies, antibody-drug conjugates) and a large number of approved therapies. For example, of the 33 new molecular entities approved so far in 2017 approvals (see here), 9 (or 27%) were biologics, of which 7 were monoclonal antibodies; one was an enzyme replacement therapy and one was an antibody-drug conjugate.
Anti-sense oligonucleotides (ASO) – A seminal discovery for ASO came in 1978, when Zamecnik & Stephenson published findings on oligonucleotide inhibition of Rous sarcoma virus replication. The first ASO was approved in 1998: fomivirsen for the treatment for cytomegalovirus retinitis. However, there was only a single ASO approved in the next 18 years (mipomersen for homozygous familial hypercholesterolemia in 2013). In 2016, two more were approved: eteplirsen for Duchenne muscular dystrophy and nusinersen for spinal muscular atrophy. The field is incredibly active, however, with dozens of clinical trials ongoing. A search for “antisense oligonucleotide” on clinicaltrials.gov returns 63 active studies; see here for Ionis development pipeline, as another example. [Throughout this blog, “active studies” is defined by the search terms “Recruiting”, “Active”, “Completed”, and “Enrolling by invitation Studies”.]
In vivo Gene therapy – It is not easy to pinpoint the exact date of the technical breakthrough that led to gene therapy. In 1972, a paper published in Science proposed that exogenous DNA be used to replace the defective DNA in those with a genetic disease. In 1984 a retrovirus vector system was designed that could efficiently insert foreign genes into mammalian chromosomes. The first clinical trial was in 1990. It was not until 2012 that gene therapy was first approved: Glybera was approved by the EMA for the genetic disease lipoprotein lipase deficiency (see here). (I am defining in vivo gene therapy as the permanent introduction of DNA into somatic cells by viral gene transfer; see below for ex vivo gene therapy.) No additional in vivo gene therapies have been approved, and none has been approved in the US, although there are hundreds of ongoing clinical trials with very promising results. A search for “gene therapy” on clinicaltrials.gov returns 2,100 active studies; see here for bluebird bio pipeline, as another example.
Ex vivo gene therapy –The distinction from in vivo gene therapy is that here, cells are extracted from a patient, purified so that only a specific subset of cells remains (e.g., CD34-expressing hematopeitc stem cells), exogenously manipulated, and returned to the patient. The first ex vivo gene therapy, Strimvelis, was approved in 2016 for a rare genetic disease called Severe Combined Immunodeficiency (SCID). This particular form of SCID is due an inherited deficiency of the adenosine deaminase gene. While no additional ex vivo gene therapies have been approved, there are now numerous tools available to genetically engineer cells (see CAR-T and CRISPR, below).
Oncolytic viruses – Oncolytic virus were first described in the 1960’s. In 2015, the US FDA approved an oncolytic virus with an abominable name, talimogene laherparepvec, (fortunately abbreviated “T-Vec” [Imlygic]), for the treatment of melanoma in patients with inoperable tumors. No additional oncolytic viruses have been approved. Research continues, however. For example, a recent publication in Science Translational Medicine described the use of an oncolytic virus that neoplastic cells in the brain (e.g., glioma), but cannot attack normal neurons (here). Therapeutically, the oncolytic virus – a recombinant poliovirus/rhinovirus chimera named PVSRIPO – may act as a potent immune adjuvant that generates tumor antigen–specific cytotoxic T lymphocyte responses.
Cellular therapy – For simplicity, I am excluding the entire stem cell transplant and organ transplant fields. There is a massive amount of experience with transplants. Here, I am solely focused on cellular therapies that require regulatory approval, as the cells themselves are manipulated ex vivo and returned to the patient (see FDA website here). The list is short, and includes products from cord blood, autologous cultured chondrocytes & fibroblasts, and allogenic cultured keratinocytes. The only other therapies on the list are, Provenge, T-VEC (oncolytic virus, see above), and Kymriah (CAR-T, see below). Provenge is a cell-based cancer immunotherapy for prostate cancer. It is a personalized treatment that works by programming each patient’s immune system – and dendritic cells in particular – to seek out cancer and attack it as if it were foreign. The term “dendritic cells” was coined in 1973 by Steinman & Cohn; the former was awarded the Nobel Prize in 2011.
Chimeric antigen receptor T cells (CAR-T) – The science behind immunotherapy dates back decades. In 2003, Dr. Carl June heard a presentation by Dr. Dario Campana of St. Jude Children’s Research Hospital. Dr. June requested a sample of Dr. Campana’s chimeric antigen receptor construct. In 2005 Campana and colleagues published their work on chimeric antigen receptors (see here). On August 20, 2017, the first chimeric antigen receptor T cell (CAR-T) therapy was approved by the FDA (see here; New York Times article here). The “drug” derives from T cells collected from each patient, re-engineered to create a receptor that targets tumor cells, and then infused back into the patient to attack cancer. Several other CAR-T therapies are nearing approval, too. A search for “CAR-T” on clinicaltrials.gov returns 324 active studies.
Other promising modalities for which there are no approved drugs:
In this section, I highlight a few new modalities, along with recent reports in the news or scientific literature which highlight the promise of each.
RNA interference (RNAi) – This is the inspiration for this blog. While not yet approved, the top-line data from Alnylam are reported as positive. Interestingly, a search for “RNAi” on clinicaltrials.gov returns only 29 active studies.
CRISPR – This gene editing technology needs no introduction. In the news this week: the prestigious Lemelson-MIT Prize was a awarded to Feng Zhang (here), and there was a nice Nature Reviews Drug Discovery interview with the CEO of Editas, Katrine Bosley (see here). The potential therapeutic application of CRISPR goes beyond ex vivo gene therapy. Indeed, organs derived from CRISPR pigs may arrive at a transplant center near you (see Science publication from Luhan Yang, George Church and colleagues here; website for their company, eGenesis, here).
mRNA therapeutics – Messenger RNA (mRNA) was discovered by Jacob, Brenner and Meselson in 1961. Decades after understanding the central dogma that DNA encodes for RNA encodes for protein, there are no approved mRNA based therapeutics. There are many in development, however, including areas such as cancer immunotherapy, vaccination against infectious diseases, and protein replacement. A study published this week describes how an mRNA-based influenza vaccine induces a type-I IFN response and leads potent vaccine-specific responses (see here). Recently, Moderna Therapeutics revealed more detail on their portfolio that (see here); a search for “mRNA” on clinicaltrials.gov returns 673 active studies.
Human microbiome – Poop is all the rage. In 2013 there were $13 million in investments disclosed in microbiome drug developers; in 2015, there was over $300 million (see here). Flagship Pioneering has been very active in the “microbiome as therapeutics” arena, including companies such as Seres and Evelo, and a new company recently announced, Kaleido Biosciences (see here). Also in the news recently: Flagship submitted an SEC filing that targets $500 million for a new fund, bringing total assets under management to $2.25 billion (see here). Only a fraction of this Flagship money will likely be invested in microbiome…but still!
Proteolysis targeting chimera (PROTAC) – This is a two-headed small molecule where one head binds to an E3 ligase (which degrades protein) and the other head binds to a substrate (which gets degraded by the E3 ligase; Nature Reviews Drug Discovery article here). An interesting report published in Cell this week describes a small molecule that acts via protein degradation (see here). While not PROTAC, it is an example of intracellular protein-mediated degradation.
And there are other examples of novel modalities on the horizon, including red blood cells as therapeutics (e.g., Rubius), neoantigen cancer vaccines (e.g., Neon), and even so-called “digital therapeutics”.
Here are a few of my takeaways.
- (1) It takes a LONG time to go from scientific discovery to an approved therapy, especially for new modalities that have not yet been tested in humans. Although this is stating the obvious for those who do drug discovery and development, it is worth saying again and again and again. Drug discovery and development is hard, even for established modalities such as small molecules, peptides and monoclonal antibodies. With new modalities, there are new risks & challenges, including “unknown, unknowns” related to off-target toxicities; path to regulatory approval; manufacturing drug product; supply chain; and commercial market.
(2) It is not important to be first, but it is important to be ready. Once the first new modality makes it through the regulatory process and the drug product gets to patients for the first time, many of the unknowns go away. Quickly, the field adapts and learns the value to patient care. Just look at monoclonal antibodies: after the first approval (muronomab), there was only one additional medicine (abciximab) approved over the next 10 years; it took another five years for the modality to become established across the biopharmaceutical industry. Today, there are very few major biopharmaceutical companies who don’t have monoclonal antibodies as part of their clinical portfolio. The important point: companies that are fast to adopt and incorporate new modalities will likely do really well. A company does not have to be first; they just need to be ready.
- (3) I feel as if we are on the cusp of breakthroughs for several novel modalities. If the pattern for monoclonal antibodies is true for other new modalities with at least one approved medicine (e.g., antisense oligonucleotides; cellular therapies such as CAR-T, oncolytic virus and ex vivo gene therapy), then the next 5-10 years should lead to the approval of multiple medicines that are considered “new modalities” today. Indeed, a search of clinicaltrials.gov indicates that there are many active studies underway. Moreover, may other modalities, such as RNAi, are will likely get approved in the near future.
(4) If new modalities are on the horizon, many “undruggable” targets may become druggable. For someone like me who spends most of their time in discovery and early development, what is incredibly exciting is how these new modalities are unlocking “undruggable” targets. I roughly estimate that only ~10% of protein targets are druggable by small molecules and monoclonal antibodies. With new modalities come new mechanisms to perturb targets. These new modalities can replace defective genes, turn-on new cellular functions, and perturb systems not just individual protein targets. As new targets and pathways are identified via human genetics and other disciplines, a drug hunter will have options from which to choose.
(5) Many new modalities have the potential to become rapidly programmable to test therapeutic hypotheses quickly in humans. This remains an aspiration of mine: to rapidly move from therapeutic hypothesis to a clinical proof-of-concept study (see previous blog here). With new modalities come the potential to rapidly program molecules to test therapeutic hypotheses. We are still a long way from this reality, but I expect we will make substantial progress towards this aspirational goal in the next 5-10 years.
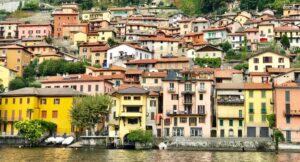
It is a time to celebrate the accomplishments of Alnylam and RNAi. It is also a time to be optimistic for all the other new modalities that are breaking ground and creating therapeutic options for patients in need. Like the colors of houses on Lake Como, Italy (photo below), it is time to move beyond a few conventional modalities to embrace a palette of options.