This week I want to focus on the role of biomarkers in drug discovery and development, which is one of the three pillars of a successful translational medicine program (see slide deck here). The focus is on Alzheimer’s disease, based on recent articles published in JAMA. At the end of the blog you will find postings for new biomarker positions in Merck’s Translational Medicine Department.
[Disclaimer: I am a Merck/MSD employee. The opinions I am expressing are my own and do not necessarily represent the position of my employer.]
Before I start, I want to point to a few blogs that provide counterarguments to some of the optimistic opinions expressed in this blog. The first is David Dobb’s negative view on big data (here); the second on Larry Husten’s concerns about conflicts of interest between academics and industry, as it relates to a recent NEJM series (here). I will not comment further, but it is worth pointing readers to these blogs and related blogs for a balanced view on complicated topics.
I have expressed the strong opinion that what ails drug discovery and development is that we pick the wrong targets, don’t develop robust biomarkers, and we don’t test therapeutic hypotheses quickly enough in clinical trials. Here, I want to highlight examples of biomarkers en route to (hopefully) successful drug development in Alzheimer’s disease. Two JAMA papers (here, here), along with a concise JAMA Editorial, describe the use of imaging and molecular biomarkers of amyloid pathology in human subjects before the development of AD. The studies used positron emission tomography (PET) imaging or the presence of beta-amyloid in cerebrospinal fluid (CSF), and correlated the presence of these biomarkers in pre-AD patients with a range of cognition [normal cognition, subjective cognitive impairment (SCI), or mild cognitive impairment (MCI)]. The articles also provide further causal support for the amyloid hypothesis in AD.
Prevalence of Cerebral Amyloid Pathology in Persons Without Dementia: A Meta-analysis, Jansen et al JAMA (May 2015). The first JAMA study estimates the prevalence of amyloid pathology based on biomarker criteria in persons without dementia. The study included amyloid PET data from 29 studies and cerebrospinal fluid (CSF) amyloid-β1-42 data from 31 studies. These imaging and molecular biomarkers were used to estimate the probabilities of amyloid positivity according to cognitive status, APOE-ε4 status, and an age range of 18 to 100 years. As stated in the accompanying JAMA editorial by Roger Rosenberg: “The central observation in this meta-analysis was that the identified risk factors for AD-type dementia are also the same risk factors for amyloid positivity in persons with normal cognition.” The Jansen et al article concludes: “These findings suggest a 20- to 30- year interval between first development of amyloid positivity and onset of dementia.” This estimated 20-30 year interval is longer than but generally consistent with the 15-25 year interval between the first evidence of CSFAβ42 decline and increase in amyloid PET positivity and symptoms in familial AD patients reported by Bateman et al in the NEJM.
Prevalence of Amyloid PET Positivity in Dementia Syndromes: A Meta-analysis, Ossenkoppele et al JAMA (May 2015). The other JAMA article extends the findings related to amyloid pathology with a meta-analysis to estimate the presence of amyloid positivity on PET in a wide variety of dementia syndromes. The authors included data involving 1359 persons with clinically diagnosed AD and 538 participants with non-AD dementia. Somewhat paradoxically (at least to me), the authors demonstrated that the prevalence of amyloid on PET decreased with age in AD-diagnosed patients, mostly with APOE-ε4 noncarriers, and increased with age in most non-AD dementias. A take-home message is that amyloid imaging may be most critical in making the correct diagnosis in early-onset dementia, especially to rule in AD dementia.
Why this is important: Applied to drug discovery and development, there are three important biomarker messages from these JAMA studies. First, longitudinal clinical studies, such as those described here, provide causal human biology support for the amyloid hypothesis. Observational studies alone on the presence or absence of biomarkers (e.g., β-amyloid) in patients with AD do not establish causality. However, if the biomarkers are present before AD onset and predict development of AD, then this provide support evidence for causality. A note of caution: longitudinal studies of β-amyloid do not provide definitive support of the amyloid hypothesis, nor do they implicate specific targets that can be modulated and thereby protect from AD. When combined with other experiments of nature (e.g., human genetics) or an elucidation of the components of the amyloid plaques, it is feasible to select specific targets for target modulation.
Second, when a biomarker is established along a causal pathway, it follows that it represents an appropriate biomarker of target modulation. The JAMA studies suggest that CSF-based biomarkers of β-amyloid levels can be measured before and after administration of a drug to make sure that the drug is doing what it should be in human subjects. Indeed, CSF Aβ42 (a surrogate for insoluble β-amyloid) levels and kinetics are used to measure target modulation in in pre-clinical non-human primate models (see here). Consistent with this model, it is interesting to note the high correlation between PET and CSF Aβ42 peptide biomarkers (concordance rates of ~90%).
And third, β-amyloid biomarkers can be used to enrich for patients likely to develop AD, and therefore enrich for patients enrolled in clinical proof-of-concept (PoC) studies. The observations from Jansen et al provide evidence for the hypothesis that amyloid positivity reflects early AD. The observations from Ossenkoppele et al suggest that amyloid imaging might have the potential to be most helpful for differential diagnosis in early-onset dementia, particularly if the goal is to rule-in AD dementia. Together, these observations suggest that an enrichment strategy for those who may benefit the most from early intervention are subjects with any combination of APOE-e4 genotype, mild cognitive impairment, and presence of amyloid by PET imaging.
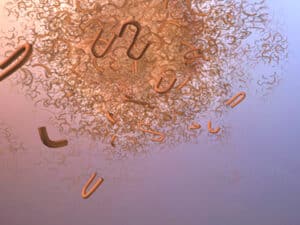
What is incredibly humbling, however, is that these JAMA studies reinforce the prevailing view that there is a 20- to 30-year interval between amyloid positivity and AD-type dementia. Furthermore, amyloid positivity does not guarantee development of AD. Thus, what is the role of amyloid in the progression to AD? The assignment of cause and effect for amyloid in AD, and for pathology in neurodegenerative diseases in general, is far from clear. Considerable evidence also links tau to neurodegeneration, which raises additional questions such as whether amyloid precipitates the spread of tau or whether amyloid deposits in reaction to the damage done. As we press towards discovering and characterizing new imaging tools to study the progression of disease-related biomarkers, such as a PET tracer for aggregated tau filaments (see here), our understanding of disease causality, our ability to identify the appropriate population for novel disease-modifying therapeutic trials, and our ability to make early biomarker-driven assessments of the potential of novel therapies will increase.
Here are positions that are available within Merck’s Translational Biomarker (tBio) Department, led by Dr. Jeff Evelhoch.
Director of MR/CT/Ultrasound/Optical group in West Point, PA.
Senior Radiochemist in the PET tracers group in West Point, PA
http://jobs.merck.com/MSD/job/West-Point-Senior-Radiochemist-Job-PA-19486/267395300/